Healthcare Self-Distribution: Early Considerations
We recently hosted a web event titled Demystifying Demand Planning: WHY and received an interesting question from one of the participants. The question had a much broader reach than Demand Planning and I thought it would be terrific to share it with all of you.
The question was, “What are the most important things to do when changing from individual hospital storerooms to a central warehouse servicing multiple locations spread out over 200 miles? We’re considering doing this. Luckily, all are on the same software system and applications right now.”
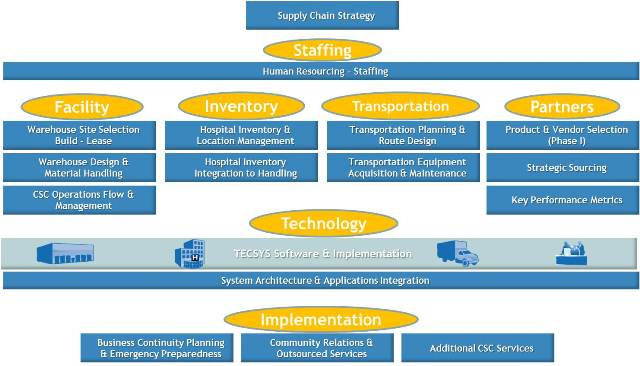
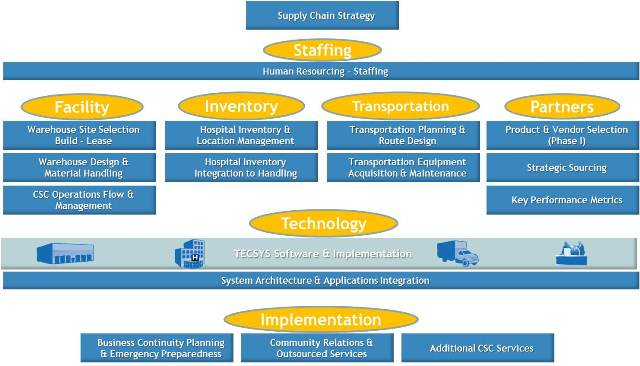
As you no doubt know, there is not a simple answer; this is a significant business undertaking! As I look at it, there are several things you need to be considering, all related, some simultaneous, some sequential. Let’s look at it as components.
- Staffing: The first, critical component. Do you have the right skillsets in place to move to this new model? Most organizations that have done this successfully talk about the importance of having expertise around SUPPLY CHAIN, not just historic Material Management. A Consolidated Service Center or Distribution Center or centralized warehouse is a whole different level of operation, and you need to have the talent in place to manage the change to a successful outcome.
- Facility: Central warehouse space and organization considerations. How do you plan to manage your supplies? Are you moving completely to self-distribution? What will be your new ordering quantities – cases, pallets? Will you also be supporting low unit of measure (LUM) distribution back to the clinical facilities? These functions will drive both the size and configuration of your warehouse. Will you be expanding your operation to include other services to the IDN, such as pharma, surgical kits, etc? If so, it is best to identify space issues now and build them into the overall plan. Once you know facility size and functions, you will look into the build, buy or lease scenarios.
- Inventory: It’s all about visibility. Overall, how much inventory is there and where is it all? Will you be transferring it all to the central warehouse or moving it into clinical areas? Either way, what is the space needed to hold it during the transition? How will your space needs evolve? In other projects of this nature we have seen an inventory reduction up to 30% right off the top, through obsolete or expiring products, so this opens up some opportunity. Let us also work from the premise that not all products are equal in the clinical setting and not all products should be replenished as they have been historically. Look, as best as possible, at true product consumption vs. ordering and start with high volume, high value products. They should be the first to be segmented, weighted, prioritized and, generally, the first to be centralized. A question for additional consideration is, How far do you want to track your inventory? Through to point of use? This is the time for you to be considering longer-term goals so you can establish the foundation now.
- Transportation: Compared to other industries, your 200 mile territory is not large, but effective route management is important to overall efficiencies. What is the plan for both receiving and distribution? What are the physical and logistical needs, including routing, scheduling, etc.? Will you be assembling LUM totes to be delivered to clinical areas? This is the time to look at the options to buy, lease or contract with a 3PL.
- Supply Chain partnerships will be examined as you address overall inventory management. As you establish new ordering patterns, you should anticipate an evolution in some of your trading partner relationships. You can leverage the data you now generate to support demand planning discussions with the manufacturers and suppliers.
- Technology: You have a good start because all your facilities are on the same system and applications. However, you will want to assess the go-forward needs, especially if you are expanding functions or if you want to track supplies to point-of-use. So, what are the technology functions you will need from both operational and data management perspectives? What interfaces would help with moving data to other areas (patient billing, BI, clinical outcomes, etc.)
- Finally, Implementation. How will you transition to the new model? Would a staged roll-out or single entire move work best for you? What are the support needs for a smooth transition? What change management tools do you need to deploy? How much training will be needed throughout the reach of your supply chain?
Two final thoughts. First, you will want to evaluate who you are partnering with through the transition. Look for partners that have expertise and can provide direction.
Finally, engage with other IDNs that have moved in this direction. In my experience they are generally open to sharing what has worked, what has been difficult, and what mitigation strategies they have put in place.